Pain free diabetes management with mHealth. Myth or Reality?

Arun Natarajan told us about the burden of type 2 diabetes and his digital tool as a solution to this
There are 4 main health problems today in the world – chronic diseases as diabetes, cancer, cardiovascular disease and rare diseases which affect an enormous number of the world population. Every 16th person in the world has diabetes. Even WHO mentioned that diabetes will be the seventh leading cause of death in 2030. This number is scary, isn’t it? Is it somehow possible to change that? What can we do now? Can we help diabetics live better lives and take care of them?
Arun Natarajan helped us to answer all these questions
Arun Natarajan is a researcher at ID GmbH & Co. KGaA and he is currently working on a concept of Painless home-based glucose monitoring device and an associated app for Type 2 Diabetics – Salivary Glucometer
Glib Kutepov: What is happening to a person when he finds out that he has Diabetes?
Arun Natarajan: Onset of stress and depression can happen because of a diabetes diagnosis. This person has a psychological burden, as he must take medications all the time and this combined with lifestyle modifications, increased financial burden. This growing psychological burden high reflects on his productivity and crucifies his life’s standards.
But once this person is reinforced holistically, he confidently controls his diabetic state, rather than diabetes controlling him. Positive reinforcement can be achieved by a multimodal approach – regularly measure and monitor sugar level, know the diet, relate the amount of exercise to the blood glucose and appropriate medication. By controlling sugar holistically rather than depending on medication alone, provides a considerable amount of positive changes in a diabetic. Digital tools for healthcare can play a major role in aiding the diabetic patient reach a point of control of his disease. New mHealth apps for diabetes management can give psychological comfort for people diagnosed with diabetes and indirectly reduces stress levels and aids in controlling blood sugar.
Glib Kutepov: What are the numbers and trends of sick people with Diabetes 1 and 2 in the world. How many diagnosed and undiagnosed?
Arun Natarajan: Type 1 is a less common form of diabetes; it makes up an estimated 5–10% of all diabetes cases. People with type 1 diabetes generally don’t produce insulin, a patient needs to inject insulin every day and daily take care of his diet and activities. Type 2 diabetes is easier to monitor than type 1. The patient does not need to go to a doctor every day, once per month is enough. Here it is important to monitor yourself, and constantly take medications. Regarding your second question, the number of people with diabetes has risen from 108 million to 422 million people worldwide, and 187 million of them do not even know they have the disease.
Glib Kutepov: What is the global cost of diabetes treatment? How much do we spend on diabetes type 1 and type 2?
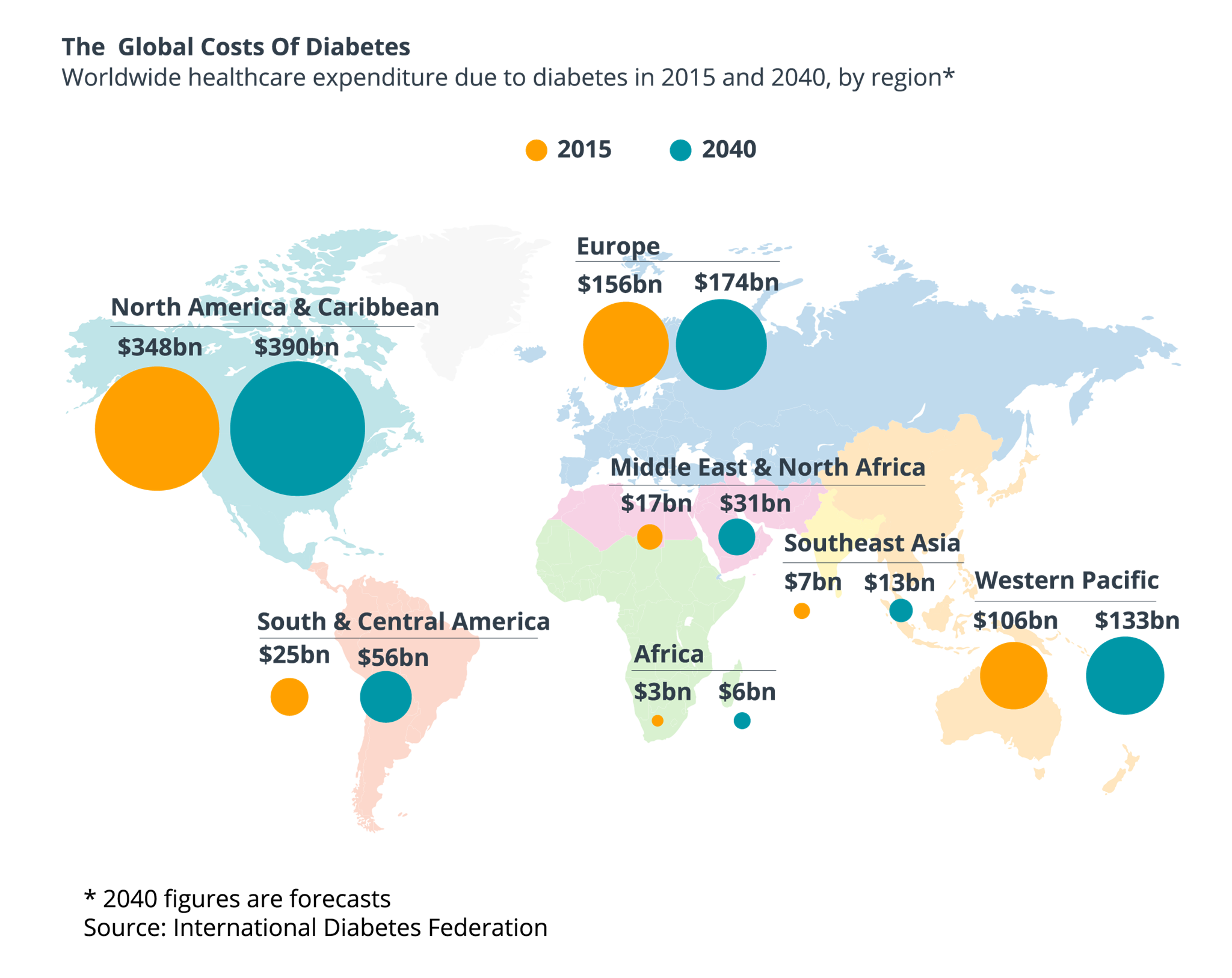
Arun Natarajan: The global cost of diabetes is now 825 billion dollars per year and this number is continuously growing. The largest cost to individual countries being in China ($170 billion), the US ($105 billion), and India ($73 billion). In men diagnosed with diabetes type 2 at ages 25-64 years, the lifetime direct medical costs were ranging from $84,000 to $124,700. In women, the costs were ranging from $85,500 to $130,800.
Glib Kutepov: How did people use to monitor themselves before the era of digital tools for healthcare?
Arun Natarajan: They used to have a small hand-written Excel sheets where they manually entered all their data. Every 6-8 weeks a patient goes to his doctor, checked himself and presented this data.
Glib Kutepov: So when the person is diagnosed with diabetes, the best case scenario for this person would be: You’re a diabetic, but here’s an app and it will take care of you, it will blink when you need to take your medicine and it will measure youк sugar level. What would be the comfort scenario for someone diagnosed with diabetes?
 Arun Natarajan: The comfort scenario is when an app makes numbers simple to understand, provides insights in human readable texts and also talks to a person and reminds him what he needs to do. We still wake up and check our Facebook feeds, why not to hear something?
Arun Natarajan: The comfort scenario is when an app makes numbers simple to understand, provides insights in human readable texts and also talks to a person and reminds him what he needs to do. We still wake up and check our Facebook feeds, why not to hear something?
Glib Kutepov: I wanted to ask you about mySugr app which was sold to Roche for 100 million. Have you heard about this?
Arun Natarajan: mySugr was a first data analytics app for patients. The user simply puts all the data in this app and the app analyzes information and gives weekly and monthly reports how the sugar is progressing. Users need to enter their data about blood sugar readings, meals and medicines.
Glib Kutepov: What was the added value of this app?
Arun Natarajan: Imagine the patient who doesn’t go to the hospital constantly, he continuously skips taking medications, and does not take care of himself. If the person is not motivated, he will not take care of himself. This app was a first self-motivator for these people, mySugr made life with diabetes easier. Person’s therapy information was just there all in one place and easy to understand.
Glib Kutepov: But you know that they sold an app for 100 million? How did it happen?
Arun Natarajan: Of course the app was simple and user-friendly, and because of this it had a considerable user base and an enormous amount of data. It’s popularity and easy to use interface combined with diabetic data considerably increased the market value of this app.
Glib Kutepov: People talk about 4 main components for effective diabetes monitoring: do exercises, know your glucose level, follow your diet and don’t stress. MySugr app follows only 1 of them, what about the remaining 3?
Arun Natarajan: MySugr was the first app to track patient's glucose data. Patients also have the options to enter other data like meals and stress levels. However, the user had to enter all the data manually. Nowadays, there are apps that automate the data collection process.
For example, GoMeal, Calorie Counter, Glucose Buddy, and GlucOracle – apps that help people to monitor and improve their food intake. In addition, these apps offer target planning and goal setting to help patients manage their caloric intake and their weight. Above all, there are digital tools that use artificial intelligence and image recognition techniques to analyze food content based on the photo of the food.
Glucose Buddy- helps you to take care of your blood glucose and medication use. Some pros of Glucose Buddy is that it allows to personalize the customer information based on a number of factors including the user's height, weight, age, gender and type of diabetes and blood glucose. It also provides a graphical depiction of blood glucose numbers with color-coded highs and lows and its features allow the user to email pictures of their graphed glucose, carb and activity results to their doctor.
Fitbit is pairing up with Dexcom, a company that creates continuous glucose monitoring (CGM) devices for people with diabetes. Dexcom's CGM devices work with a sensor that sits just under the skin and measures a person's glucose levels every few minutes and provides an analysis of where their glucose levels are and where they're heading. It can also be connected to Apple Watch, what creates a great user experience. The main cons of this app is that it’s very costly - $300 and the Dexcom sensor itself costs $900.
Glib Kutepov: Can you tell us more about the use of artificial intelligence in digital tools for healthcare?
Arun Natarajan: There are many companies in a healthcare sector that are currently looking into artificial intelligence and especially image recognition. One of such examples are the companies AVA and Calorie Mama. The concept of these apps is simple, you make a picture of your food, a neural network in the backend recognizes the meal type and matches it with the nutrition database to extract the amount of sugars in your food. The main idea behind it is that people love taking pictures, so why not calculate the number of calories of your food and stay healthy? Such apps with artificial intelligence will become a great help for diabetes, as they would be able to track food intake with less fuss.
Glib Kutepov: Is there a healthy balance between enjoyment and health? What can be better than eating a juicy hamburger and a pint of beer on Friday evening?
Arun Natarajan: There’s a funny quote: “Either you die healthy or die happy.” It’s your choice. We need to strike a deal between the health and enjoyment and neither of them should affect one another.
Glib Kutepov: What kind of diseases can you imagine in 2050? What would be left?
Arun Natarajan: Cancer can be the first big villain because of more consumption of GMOs and chronic exposure to chemicals. As our life is changing, it is now coupled with a sedentary lifestyle and excessive stress, so, the next big fish in the bucket will be lifestyle-related diseases like hypertension and diabetes.
Glib Kutepov: Do you think that digital tools for healthcare can change people’s lives in the future?
Arun Natarajan: Sure! Modern apps can help you take a full control of your health, they care for you, provide you the detailed timelines, graphical insights of any patient’s health data. I think digital healthcare is the least tapped of all the fields IT has stepped in.
Glib Kutepov: Arun, let’s talk about your project - Salivatary Glukometer. How did you come up with an idea to measure sugar level in saliva?
Arun Natarajan: My father is a Type 2 Diabetic and most days he skips his medication. He used to avoid routine self-monitoring of his blood sugar reason. Soon I realized the reason for his disinterest in self-care of his diabetic state was the fear of pain he had to experience to undergo a blood test. This avoidance attitude left him extremely unmotivated to follow his proper regimen of medication, diet, and exercise. I understood it was a vicious cycle which was initiated by the fear of pain.
300 solutions on a market to make tests based on a blood, but did we ask anyone if they would like to prick themselves every time? Probably not! This painful prick induces an immense amount of stress for the patient and most patients tend to skip home monitoring at times for the fear of the prick.
Studies have shown that saliva can be used as a substitute for blood to assess the amount of glucose in a diabetic. Obtaining a salivary sample is easy compared to getting a blood sample – a spit compared to a prick. The main difference of these two is that saliva, not blood. Moreover, the cost difference of using Salivary Glucometer and Blood Glucose Meters is tremendous. Blood Glucose Meters require to purchase test strips, which a diabetic patient could use up to 12 times a day and the cost of one strip can be up to $8. Salivary Glucometer requires only one strip and the cost of it is ranging from $2-$5.
Salivary Glucometer is a blood monitoring device that is simple, painless and stress-free. This will not require much technological knowledge to use the device. The smartphone app will also have a simple user interface which will be comprehensible by all users. The app will be able to integrate data from other mHealth apps, diet, and exercise monitoring apps and it will provide a holistic approach for the patient to relate his blood glucose to his diet and exercise.
Glib Kutepov: A very interesting concept! So what’s your plan? You want to make it and become a millionaire?
Arun Natarajan: It’s not about money, it is about solving a problem and improving the life of a diabetic and let him realize that he too can lead a normal and healthy life. That is what is most important!